SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.
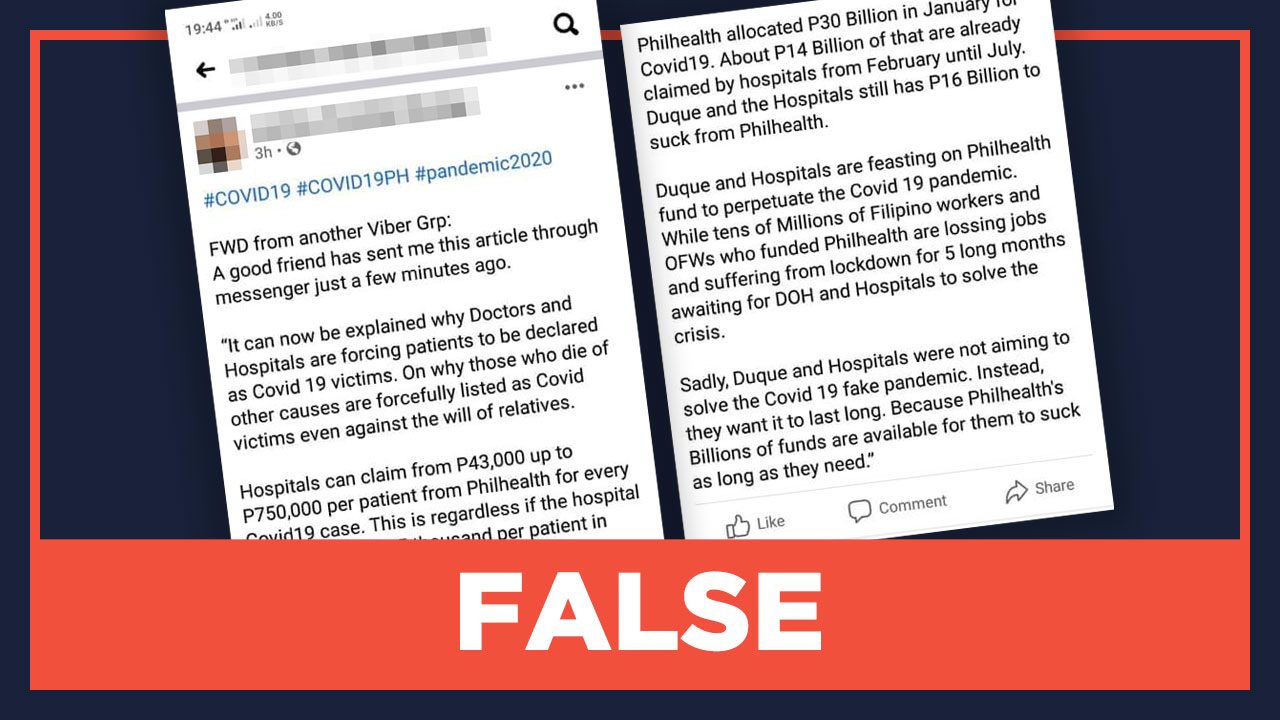
Claim:
Hospitals can claim between P43,000 to P750,000 in benefits from PhilHealth for every COVID-19 patient admitted, regardless of the actual cost of treatment.
This claim, which circulated through private messages, blamed this policy for the over-reporting of COVID-19 cases and deaths. It also accuses doctors of forcing patients to be declared as COVID-19 victims even against their or their relatives’ will.
This claim was posted on the Facebook page “Fact-checking in the Philippines” for verification.
Rating: FALSE
The facts:
Hospitals will only receive the cost declared in the COVID-19 in-patient’s itemized billing statement. The scope and limitations of PhilHealth’s COVID-19 benefit packages are indicated in Circular No. 2020-0009.
The claim that is circulating says: “Hospitals can claim from P43,000 up to P750,000 per patient from PhilHealth for every COVID-19 case. This is regardless if the hospital only spent even P5,000 per patient in treatment.”
PhilHealth does offer benefit packages between P43,997 and P786,384 for COVID-19 cases, depending on the severity of the case and the kind of hospital that can deal with the indicated severity. However, the total amount that can be reimbursed is limited to the amount indicated for each severity and its corresponding healthcare provider category. The packages are the following:
- Mild pneumonia – P43,997
- Moderate pneumonia – P143,267
- Severe pneumonia – P333,519
- Critical pneumonia – P786,384
The packages are based on pneumonia because this respiratory illness is the complication of COVID-19, according to former PhilHealth president and CEO Ricardo Morales.
Even if the total cost is less than the total benefit package, hospitals will only receive the amount that is indicated in the patient’s bill. Philhealth requires healthcare providers to submit an itemized billing statement, including professional fees, to file a claim for reimbursement.
PhilHealth’s circular also states that mandatory deductions such as senior citizen discounts and persons with disabilities discounts will be deducted from the total hospital bill and must be indicated in the itemized billing statement.
These packages are only available for Filipino patients with probable or confirmed cases of COVID-19. Probable cases are suspect cases whose tests are inconclusive, or those who underwent testing but not at an officially accredited laboratory, or who could undergo testing for any reason. Confirmed cases are patients who are laboratory-confirmed for COVID-19 through a test conducted at an officially accredited testing facility.
There also is no proof or official reports that doctors and hospitals are forcing patients to be declared COVID-19 positive. – Christine Okubo, Vernise Tantuco/Rappler.com
Add a comment
How does this make you feel?





There are no comments yet. Add your comment to start the conversation.