SUMMARY
This is AI generated summarization, which may have errors. For context, always refer to the full article.

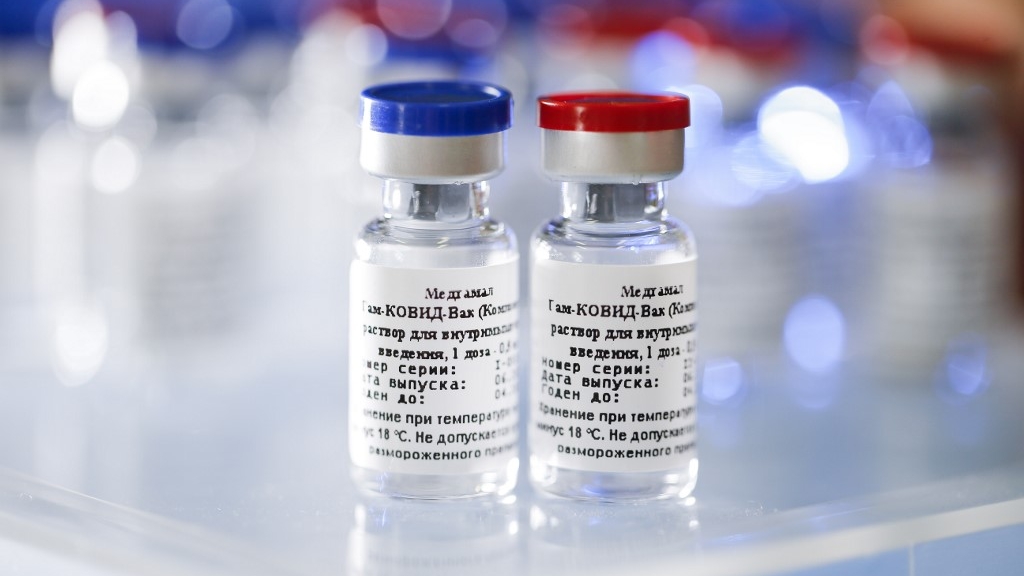
On Tuesday, August 11, Vladimir Putin announced Russia was the first country to register a vaccine offering “sustainable immunity” against SARS-CoV-2, the virus that causes COVID-19.
Developed by the Gamaleya Research Institute in Moscow, it’s been registered with the Russian Health Ministry and approved for emergency use only.
But there are concerns it will soon be rolled out across the Russian population, far beyond emergency use. This has prompted discussion about the “race” towards a COVID-19 vaccine.
While speed is important, ensuring a vaccine is effective and safe is much more critical. The consequences of doling out a potentially unsafe and ineffective vaccine could be wide-reaching.
Data about the trials has not been published
The Gamaleya Research Institute announced it registered a SARS-CoV-2 vaccine with the Russian Health Ministry, the local regulatory body that determines which medicines can be used in Russia. This vaccine is called “Sputnik V” and the Institute has indicated it’s approved for emergency use. An emergency use approval generally means a vaccine could be offered to people at very high risk of infection, such as health-care workers, but not the general civilian population.
The Institute had previously registered this vaccine for a Phase I/II trial (to assess safety and immune responses in humans), initially with just 38 people. Senior Russian officials said it induced a strong immune response and no “serious complications” in this trial. This isn’t too surprising, as published data from human clinical trials for other similar vaccines have shown strong immune responses and no serious complications.
However, the data from the trial of Sputnik V has not been published and there is no data that indicates the vaccine would actually protect, as Phase III studies (requiring thousands of volunteers to demonstrate efficacy and detect rare side-effects) haven’t been performed.
The Institute did announce a Phase III trial for Sputnik V will begin on August 12 in Russia and several other countries. However, many scientists (including Russian researchers) expressed concern the vaccine will soon be used in large civilian vaccination campaigns, which wouldn’t usually be the case with an approval for emergency use.
What are the risks
If we go back to the analogy of a “race”, we should stop thinking of vaccine development as the 100-meter sprint. Instead, think of it more like the pentathlon. In the pentathlon, each section the athlete completes contributes to their overall score and cannot be missed. If we try to run this race against COVID-19 without each section, we could end up with a vaccine which has not been properly tested, which could be unsafe and would be unethical. And then we all lose.
The risks of advancing into mass vaccination without proper testing are significant. If a vaccine is released but side-effects emerge, the consequences include both the health impacts and deterioration in trust from our community. If the vaccine does not protect individuals from infection, those who have been vaccinated could falsely believe they are protected.
Our system of methodical series of clinical trials has been designed, oftentimes with hard-won lessons, to avoid oversights and build essential data on safety, immunity and protection with vaccines.
As stated by the US Health and Human Services secretary, Alex Azar: “The point is not to be first with a vaccine. The point is to have a vaccine that is safe and effective for the American people and the people of the world.”
Development takes time and we need to be realistic with our timelines and expectations.
Testing a vaccine is rigorous
When countries consider introducing a vaccine, the following information is examined:
- how safe is the vaccine?
- how well does the vaccine work?
- how serious is the disease the vaccine would prevent?
- how many people would get the disease if we did not have the vaccine?
This information is collected during each phase of the clinical trials (Phase I, II and III), with a particular focus on vaccine safety at each step. Developing this package of information can take years, but there have been cases when timelines were condensed.
For example, testing for an Ebola vaccine was condensed down to 5 years due to a critical need for a vaccine in the midst of ongoing epidemics. Regardless of this urgency, each clinical trial phase was still completed.
Phase III clinical trials are especially critical to assess safety in a large group of people, because certain rare side effects may not be identified in earlier, smaller trials. For example, if a vaccine-related side effect only occurred in one in every 10,000 people, the trial would have to enrol 60,000 volunteers to detect it.
In general, vaccines are more thoroughly tested than any other medicine. We administer vaccines to healthy people, so safety is the key priority, and we administer vaccines to large numbers of people, so rare side-effects must be identified.
What’s in this vaccine?
This type of vaccine is called a viral vector. With viral vectors, we trick our immune system with a bait-and-switch; we take a harmless virus, modify it so it can’t replicate, and include a target from the surface of the SARS-CoV-2 virus. The vaccine looks like a dangerous virus to the immune system, so the immune response is relatively strong and targeted against SARS-CoV-2, but the virus can’t cause disease.
Sputnik V is unusual because it uses two different viral vectors, one after the other, in what we call a “prime boost”. The first is called Ad26, which is similar to a COVID-19 vaccine being developed by Johnson&Johnson, and the second is called Ad5, which is similar to a COVID-19 vaccine being developed by CanSino Biologics. This prime boost should generate a relatively strong immune response, but we don’t know for sure.
Viral vectors are also a relatively new technology. There have been a number of large clinical trials with viral vectors for HIV, Malaria, Tuberculosis and Ebola, but only one for Ebola has ever been approved for use in the general population. – The Conversation|Rappler.com
Dr Kylie Quinn is an RMIT University Vice-Chancellor’s Research Fellow and leads the new Ageing and Immunotherapies Group.
Dr. Holly Seale is a Senior Lecturer at the School of Public Health and Community Medicine and the Program Co-Director of the Master of Infectious Diseases Intelligence course of UNSW.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Add a comment
How does this make you feel?




There are no comments yet. Add your comment to start the conversation.